Newborn babies tested for over 200 genetic conditions


Hundreds of babies have begun to be tested for over 200 rare genetic conditions as part of a world-leading study that has now launched at Leeds Teaching Hospitals NHS Trust (LTHT).
The pioneering study aims to identify conditions such as Metachromatic leukodystrophy (MLD) in babies sooner, and could enable hundreds to benefit from earlier diagnosis and treatment that could help slow the progression of disease and improve or even extend their lives.
The Generation Study, led by Genomics England in partnership with NHS England, sees newborn babies offered whole genome sequencing using blood samples which are usually taken from their umbilical cord shortly after birth.
The sequencing identifies treatable, rare conditions shortly after a baby is born rather than when symptoms might appear later in childhood. This means families can access the right support, monitoring, and treatment from the NHS much earlier for these conditions.
The Generation Study will identify more than 200 conditions in otherwise asymptomatic babies where symptoms might not present until later in childhood. Early effective intervention can help to prevent longer term health problems associated with certain conditions, keeping children out of hospital, and helping them live healthier lives.
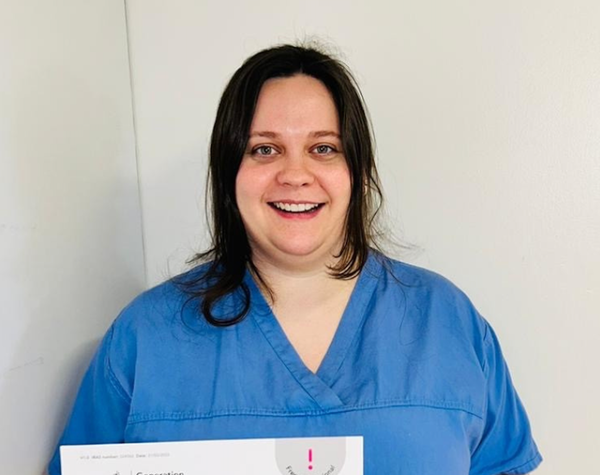
The first person to be recruited in Leeds was Georgie, who is expecting her first baby in April. Georgie is a midwife on the delivery suite at St James’s Hospital and explained why she signed up to the Generation study:
“As midwives, we see every day how research makes a difference to the care we provide, so I didn’t hesitate to sign up. Having the test will hopefully give me peace of mind when my baby is born and help future generations too.”
The very first baby to have their cord blood tested in Leeds was Suvansh, born on 4 December by Caesarean section. In a twist of fate, it was midwife Georgie who took the cord blood sample for the Generation study!
Suvansh’s mum Sonalika said:
“It was important to us to sign up so that we can find out about any problems and get treatments earlier so that my baby can have a longer, healthier life. We know we will be supported by the hospital if anything is found when we get the test results. We are very grateful to midwife Georgie and all the maternity team for their care and kindness after Suvansh’s early arrival. The neonatal unit have also been amazing and looked after us very well.”
Expectant parents are informed about the study during pregnancy, and if interested a research midwife will have a detailed conversation with them to decide if they want to take part.
Shortly after birth, an NHS doctor or midwife will confirm with parents that they are still happy for their baby to be tested and a blood sample will be taken and sent to a laboratory for whole genome sequencing.
Results are then reviewed by NHS genomic scientists, with the aim of sharing with parents within 28 days if a condition is suspected or within a few months if no conditions are suspected.
If a newborn baby is identified as having a treatable childhood condition through the genome sequencing, families and carers will be provided with further NHS testing to confirm a diagnosis, and ongoing support and treatment from the NHS.
Mr Nigel Simpson, principal investigator for the Generation study and Consultant Obstetrician at LTHT, said: "The Generation study is incredibly exciting for the future care of babies and offers a fantastic opportunity now for families to access free testing. I would urge anyone who is pregnant to take a look at the Generation website and register their interest. Our research midwives are always happy to answer any questions and support expectant mothers to join the study."
Amanda Pritchard, NHS chief executive, said: “Diagnosing rare conditions in newborn babies at the earliest opportunity through genomic testing could be truly life-changing for families – it has the potential to give thousands of children the chance to access the right treatment at the right time, giving them the best possible start to life, and for families to better plan for their care.
“The NHS is a world leader in genomics, and this study demonstrates the benefit of our partnership with Genomics England – allowing us to deploy cutting-edge technology to improve patients’ lives. If we can diagnose and treat children for rare genetic conditions years earlier, we have the power to help stop debilitating conditions in their tracks and enable more children to grow up, start school and live independently – this will be transformational for patients and for the future of medicine.”
Every year, thousands of children are born in the UK with a treatable rare condition with genetic testing usually taking place in the NHS Genomic Medicine Service when the child has developed symptoms – with children under the age of five disproportionately affected.
The NHS blood spot screening (the heel prick test) is used to detect nine rare but serious health conditions in newborn babies – the Generation study is not intended to replace routine screening, and it is important that whatever decision parents make about participation in the Generation Study, their baby still has the blood spot test.
It is hoped that screening a baby’s entire genome – all of their DNA – could detect hundreds more rare, treatable diseases in their first years of life.
Dr Rich Scott, chief executive officer at Genomics England, said: “The launch of the Generation Study is a pivotal moment as we look to develop evidence on whether genomic newborn screening should be offered to all children – to do more for the thousands of children born every year in the UK with a treatable genetic condition.
“Children with these conditions often go years without receiving a diagnosis. Cutting this time would mean earlier access to what can be life-changing treatment. The Generation Study also shows the impact of our partnership with the NHS – meaning that the UK is uniquely placed to test, and – where proven – roll out genomic innovations to improve health and help us move healthcare increasingly to preventing illness.”
NHS teams will also provide families with advice on how to manage different conditions, for example one of the conditions, osteogenesis imperfecta, parents can be advised on handling of their newborn to prevent long-term damage to their child's bones.
The study will support broader healthcare research to improve testing and discover more treatments and explore the potential of storing an individual genome over a person’s lifetime and using it to help predict, diagnose and treat future illnesses.
For example, if a child who has had their genome sequenced falls sick when they are older, there may be an opportunity to use their stored genetic information to help diagnose and treat them.
The Generation Study has been developed following extensive consultation with the public, parents and families affected by rare conditions as well as healthcare professionals, policy makers and scientists. Genomics England is owned by the Department of Health and Social Care.